|
Gastrointestinal Disorders in the GSD and Several
Other Breeds
by Fred Lanting Copyright
1990, 2003
Vomiting and gastritis
— Vomiting comes easily to dogs. Grass eating and
subsequent vomiting give rise to all sorts of
explanations, the most popular being that the dog
was sick and ate the grass to help him throw up.
Actually, excess grass is more likely the reason for
the reflex action. Dogs mostly eat grass because
they like the taste of it, just as with the case of
garbage, but it does appear that individuals learn
that too much can cause vomiting, so the intentional
eating of grass to induce vomiting may come after
experience. Gastritis, an inflammation of the
stomach lining, can be caused by the ingestion of
too much grass, garbage, or indigestible materials.
It can also be caused by viral or bacterial
invasion, but much more common, especially in pups,
is the presence of endoparasites: tapeworms,
roundworms, hookworms, whipworms, and coccidia.
Actually, tapeworms or roundworms can fill up the
belly to the extent that they back up and cause
vomiting from sheer bulk. The initial treatment for
gastritis or vomiting may be the withholding of food
and administration of Kaopectate every four hours.
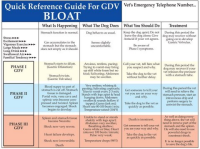
Torsion
— Commonly called bloat, sometimes described as
gastric dilation/volvulus (GDV), this is a terrifying and
frequently fatal disorder that German Shepherds and
many other deep chested dogs experience. A twisting
of the entrance and exit to the stomach traps the
food and gas. As the stomach swells, the twist is
more unlikely to be relieved without veterinary
help. Great strides in surgical treatment have been
made, but the key to reducing the high mortality is
still time. Recognize the symptoms and get the dog
to a veterinary surgeon, preferably an emergency or
trauma-oriented hospital. Simple dilation (swelling
due to gas) may not be serious as long as the dog is
able to pass food into the duodenum, but it has been
estimated that 80 percent of all dogs that
experience simple dilation will someday also have
torsion.
Symptoms of torsion
include a swollen, turgid abdomen; the sluggish
action of the dog; his white, frothy, unsuccessful
attempts at vomiting; and perhaps his scratching in
the dirt to make a cool hole in which to lie down.
Also, the spleen will feel like a hard lump. The
spleen is normally wrapped around some of the
stomach and therefore splenic torsion usually
accompanies gastric torsion, sometimes occurs
without stomach torsion. When either happens, the
return of the blood that flows through the spleen is
shut off, causing shock, the “immediate” killer.
The first thing your
vet is likely to do is attempt to push a tube down
the throat into the stomach so the gas pressure can
be relieved. If he cannot get past the twisted part
of the alimentary canal, he may opt for immediate
surgery so he can untwist the organs. One emergency
veterinary service in the Detroit area uses a
different kind of lavage tube in their treatment of
acute torsion. The large diameter, stiff, black
polyethylene pipe has a smaller, flexible tube
inserted into it. This smaller tube is for warm
water so that the stomach contents can be flushed
out of the larger one for about fifteen minutes. In
either case, once the dog has been stabilized,
decisions can be made about whether to operate, or
untwist a stomach or spleen still in volvulus.
Follow up surgical
techniques are numerous, but perhaps the one with
the most success in preventing future torsion is a
tube gastrostomy. In this procedure, a rubber or
vinyl tube is put into the stomach through the
abdominal wall, and in a week the stomach wall at
that point becomes attached with scar tissue to the
peritoneum and abdominal wall. The tube is then
pulled out. The surgical opening seals off in a few
days, and since the stomach is fused to the
abdominal wall, it is prevented from again twisting
out of position. Regular gastroplexy, which is
suturing the stomach to the abdominal cavity, is
also widely performed. Because of these and other
techniques, especially the rise of emergency
clinics, the mortality rates among those that make
it to the clinic while still alive has plummeted to
about 15 percent. Another 15 percent or so die
without being seen by the vet first.
Groups of scientists
at many locations have been studying bloat for a
long time, partly with help from such as Morris
Animal Foundation, the GSDCA, and many others. So
far, they have identified a number of likely
causative factors, including behavioral traits.
Breed susceptibility is pretty obvious, with 25
percent or more of Great Danes, Saint Bernards,
Weimaraners, and Irish Setters expected to suffer
from bloat sometime during their lives. German
Shepherd Dogs, Standard Poodles, Collies, and Gordon
Setters are fairly high on the incidence lists,
also. Some of the characteristics seen most often in
dogs that had bloated include some stressful event,
even minor, in approximately the eight hours prior
to the incident, a fearful temperament, and
consumption of fairly large quantities of non-food
material. The only dogs I’ve had direct contact with
that bloated were of impeccable character, but those
may have been in the minority. Purdue researchers
found no pattern in presoaking dry food or not, but
a slight correlation between several smaller meals
and less bloat. Others found no relation to soybean
meal in the food, an early target of breeders
looking for a primary cause. Adding vegetables and
canned or meat scraps appears to help lower
incidence. Most dogs (60%) bloated not immediately
after vigorous exercise soon after a meal, but in
mid- to late evening when resting or sleeping.
Less likely are other
types of torsion, but they can be as
life-threatening. Splenic torsion can occur without
gastric twisting, and an even more rare disorder is
mesenteric root torsion. The mesentery is the white,
fibrous, web-like or film-like tissue that connects
the various sections of intestines to each other and
to the abdominal wall. Blood vessels travel through
the mesentery, and if there is a twisting there,
regardless of whether the intestine itself is closed
off, the blood supply can be halted and the
intestinal tissue can become necrotic. Bloody
diarrhea, vomiting, abdominal swelling and/or pain,
and shock or general collapse can be symptomatic. It
may be the same as what some call “twisted
intestines”. So few dogs survive that it is
impossible to prevent recurrence or conclusively
predict whether those are at greater risk for
another attack than any other dog is.
There is a familial
element in torsion/volvulus in many, similar to the
way cancer “runs in families”, but most cases don’t
give a clue to hereditary factors. As in “toxic gut
syndrome” which is also seen a lot in some GSD
lines, it is almost impossible to tell which came
first, the presence of abnormal bacterial
populations and irritated intestinal or stomach
linings, or the bloat itself. Which is cause and
which is effect is not going to be easy or even
possible to determine. Some investigators suspect
that breeders may be stuffing their small, young
puppies’ stomachs too much, with results that show
up only later in life. Work goes on. Dr. Larry
Glickman and his group at Purdue University as well
as others have published several papers on this
syndrome. Dr. Glickman commented that the supposed
claim that raised bowls are correlated with
increased incidence in torsion/bloat may just mean
that this allows a dog to swallow more food (and
air?) more quickly than if they were on the floor. A
couple of website references, such as
<http://www.vet.purdue.edu/epi/bloat.htm>, had some
info, including from JAVMA’s Nov 15, 2000 issue. An
abstract follows:
Canine Gastric
Dilatation-Volvulus (Bloat)
School of Veterinary Medicine, Purdue University,
West Lafayette, IN 47907-1243
Non-dietary risk factors for gastric dilatation-volvulus
in large and giant breed dogs. Lawrence Glickman,
VMD, DrPH; N.W. Glickman, MS, MPH; D.B. Schellenberg,
MS; M. Raghavan, DVM, MS; T. Lee, BA
Summary of findings (references 1 & 2) -A 5-year
prospective study was conducted to determine the
incidence and non-dietary risk factors for gastric
dilatation-volvulus (GDV) in 11 large- and
giant-breed dogs and to assess current
recommendations to prevent GDV. During the study, 21
(2.4%) and 20 (2.7%) of the large and giant breed
dogs, respectively, had at least 1 episode of GDV
per year of observation and 29.6% of these dogs
died. Increasing age, increasing thorax depth/width
ratio, having a first degree relative with a history
of GDV, a faster speed of eating, and using a raised
feed bowl, were associated with an increased
incidence of GDV. Table 1 summarizes the magnitude
and direction of GDV risk associated with having
each of these factors. The relative risk (RR)
indicates the likelihood of developing the disease
in the exposed group (risk factor present) relative
to those who are not exposed (risk factor absent).
For example, a dog with a first degree relative with
a history of GDV is 1.63 times (63%) more likely to
develop GDV than a dog without a history of GDV. As
another example, if dog ‘A’ is a year older than dog
‘B’, then dog ‘A’ is 1.20 times (20%) more likely to
develop GDV than dog ‘B’.
|
Risk Factor |
Relative Risk |
Interpretation
|
|
Age |
1.20 |
20% increase in risk for
each
year increase in age |
|
Chest depth/width ratio
(1.0 to 2.4) |
2.70 |
170% increase in risk for
each
unit increase in chest
depth/width
ratio |
|
First degree relative with
GDV
(yes vs. no) |
1.63 |
63% increase in risk
associated
with having a first-degree
relative
with GDV |
|
Using a raised feed bowl
(yes vs. no) |
2.10 |
110% increase in risk
associated
with using a raised food
bowl,
contrary to popular opinion! |
|
Speed of eating (1-10 scale)
[for Large dogs only] |
1.15 |
15% increase in risk for
each
unit increase in
speed-of-eating
score for large dogs |
|
Most of the popular
methods currently recommended to prevent GDV did not
appear to be effective, and one of these, raising
the feed bowl, may actually be detrimental in the
breeds studied. In order to decrease the incidence
of GDV, we suggest that dogs having a first degree
relative with a history of GDV should not be bred.
Prophylactic gastroplexy appears indicated for
breeds at the highest risk of GDV, such as the Great
Dane.
OBJECTIVE: To identify non-dietary risk factors for
gastric dilatation-volvulus (GDV) in large breed and
giant breed dogs. DESIGN: Prospective cohort study.
ANIMALS: 1,637 dogs 6 months or older, of the
following breeds: Akita, Bloodhound, Collie, Great
Dane, Irish Setter, Irish Wolfhound, Newfoundland,
Rottweiler, Saint Bernard, Standard Poodle, and
Weimaraner.
PROCEDURE: Owners of dogs that did not have a
history of GDV were recruited at dog shows, and the
dog’s length and height and the depth and width of
its thorax and abdomen were measured. Information
concerning the dog’s medical history, genetic
background, personality, and diet was obtained from
the owners, and owners were contacted by mail and
telephone at approximately 1-year intervals to
determine whether dogs had developed GDV or died.
Incidence of GDV, calculated on the basis of
dog-years at risk for dogs that were or were not
exposed to potential risk factors, was used to
calculate the relative risk of GDV.
RESULTS AND CLINICAL RELEVANCE: Cumulative incidence
of GDV during the study was 6% for large breed and
giant breed dogs. Factors significantly associated
with an increased risk of GDV were increasing age,
having a first-degree relative with a history of GDV,
having a faster speed of eating, and having a raised
feeding bowl. Approximately 20 and 52% of cases of
GDV among the large breed and giant breed dogs,
respectively, were attributed to having a raised
feed bowl.
Another article based
on the same research but with slightly different
data pulled out for the particular subject matter,
was published in 1997: Multiple risk factors for the
gastric dilatation-volvulus syndrome in dogs: a
practitioner/owner case-control study (by): Glickman
LT, Glickman NW, Schellenberg DB, Simpson K, Lantz
GC. JAAHA, May-Jun., 1997. ABSTRACT: A study was
conducted of 101 dogs (i.e., case dogs) that had
acute episodes of gastric dilatation-volvulus (GDV)
and 101 dogs (i.e., control dogs) with non-GDV-related
problems. The control dogs were matched individually
to case dogs by breed or size, and age. Predisposing
factors that significantly (p less than 0.10)
increased a dog’s risk of GDV were male gender,
being underweight, eating one meal daily, eating
rapidly, and a fearful temperament. Predisposing
factors that decreased the risk of GDV significantly
were a “happy” temperament and inclusion of table
foods in a usual diet consisting primarily of dry
dog food. The only factor that appeared to
precipitate an acute episode of GDV [in their
observations] was stress.
This contradicted the
early-1990s study that indicated the opposite: that
raised bowls should reduce the incidence of
torsion/bloat. An article in “Bloat News” indicated
a possible link that raised feeders might help
prevent future episodes in a dog susceptible to
“aerophagic” bloat (linked to swallowing too much
air with the food, a commonly blamed cause at the
time. Another issue of the same periodical indicated
the single highest correlating factor was morphology
(body type). A graph showed a sharp incidence
increase as the depth of the chest exceeded its
width and a strong correlation with body condition
and temperament (weak nerves vs. calm, unstressed
dogs). It may be good to select dogs that have
strong, calm nerves, and are not slab-sided!
An article on the
Foster and Smith Pet Education site, “Interpret
Findings of a New Study on Bloat (Gastric
Dilatation/Volvulus - GDV) with Caution”, December
2000, at:
<http://www.peteducation.com:80/article.cfm?cls>,
starting with a subheading, “The Question of Raised
Food Bowls” circulated among fanciers. An excerpt:
“In this study, when analyzing the association
between the rate of GDV and the height of the food
bowl some questions arise. First, the study found
that large breed dogs whose food bowls are not
elevated have the lowest risk of GDV. A confusing
finding is that large breed dogs who have their bowl
raised over 1 foot have the next lowest risk, and
those who have their food bowl raised somewhere
between the floor and one foot have the highest
risk. So, the risk of GDV is not proportional to the
height of the food bowl. If height of the food bowl
is important, why doesn’t the risk steadily
increase, the higher the food bowl is raised?
Secondly, it appears that the researchers did not
consider the height of the animal in relationship to
the height of the bowl when looking for an
association between food bowl height and prevalence
of GDV. It would be of interest to compare the
height of the bowl to the height of the dog, since
dogs in this study varied widely in height due to
breed differences and age (some were only 6 months
old).
The third question is,
‘why weren’t similar findings obtained in giant
breed dogs?’ In giant breeds, dogs with food bowls
raised less than one foot had the same incidence of
GDV as those dogs who did not have their dishes
raised at all. Finally, it is unclear if the
researchers also analyzed whether the elevated
feeders were being used because other medical
problems were present or if the elevated feeders
could influence other factors such as the speed of
eating. Could these medical problems or other
factors, rather than the elevated feeders, have
contributed to the increase in GDV in this group? A
second subheading was ‘Comparison to Other Studies’:
The results of this study agree with most previous
studies, which also found that GDV increases with
age. On the other hand, in several studies, dogs who
ate faster had higher rates of GDV. In this study,
we had a peculiar finding: eating at a fast rate was
associated with an increased rate of GDV in large
breed dogs, but a decreased rate in giant breed
dogs. There have been other contradictory findings
in research on GDV. In some studies it was found
that overweight dogs had higher rates of GDV, and in
other studies, lean dogs had higher rates. In this
study, weight did not seem to make a difference. In
most studies, including this one, the rate of GDV
between males and females were similar; in one
study, however, males had an appreciably higher
rate.”
One other item that
was brought to light on a “VetMed” e-mail discussion
list, was that there is no proven advantage to
raised feeders, and that the Foster and Smith
company which runs the Pet Education website sells
many types of elevated feeders.
While some excellent
work on GDV has been carried out at Purdue, some
feel that very little research has been done in the
US on canine torsion/volvulus. Here are websites I
was told will give information on GDV; I have not
checked these out, so I cannot verify their
usefulness. Some may be “foreign links, as well as
human links and livestock links” as the person who
gave me this list said:
http://www.editoraguara.com.br/cv/ano5/cv29/cv29.htm#tormes
http://www.vetinfo.com/dbloat.html#MesentericVolvulus
http://www.canismajor.com/dog/bloat.html
http://www.harkleen.com/Chimo.htm
http://search.atomz.com/search/?sp-q=mesenteric&sp-a=000608a5-sp00000000
http://www.emedicine.com/emerg/topic311.htm
The huge retrospective epidemiological study of GDV,
as I mentioned above, is at Purdue, run by Larry
Glickman.
http://www.vet.purdue.edu/epi/bloat.htm The
project was funded by the AKC Health Foundation and
by breed clubs.
****************************************************************
Pancreatic Disorders
—Very close to where the stomach empties its
contents into the small intestine, ducts contribute
secretions from the gall bladder and pancreas,
mostly to aid in the metabolism of fats, which are
fairly resistant to action by gastric acid. If
either gland does not function properly, this can
result in loose stools, and inefficient absorption
of nutrients with highly variable severity.
The pancreas is a
rather long, V-shaped gland located near the
stomach, and aids the digestion of food. It has two
major types of cells or tissues. One group is
endocrine in nature, which means it secretes
hormones into the circulatory system, which in turn
transports them to other glands and body parts. The
endocrine activity of this gland serves to control
blood sugar level, and when defective, results in
diabetes. The other part empties a group of
biochemicals into the digestive tract. It produces
enzymes and bicarbonate, and excretes these into the
duodenum. One major enzyme, amylase, breaks down the
long starch macromolecules, while others break down
fats and proteins. Most GSD people, in America, at
least, are concerned more with the digestive
function than with diabetes. I have corresponded
with fanciers in England who are concerned about
pancreatic insufficiency, and since many of their
lines are from recent German imports, this is
possibly a more widespread problem there than I had
earlier suspected.
Clinical pancreatitis
— The word clinical may be used to mean “frank” or
“obvious”, at least to a veterinarian with the
training and equipment. Any disorder with “-itis” on
the end refers to an inflammation. Most causes of
this disorder are of unproven origin, but “bad
genes” must be the prime suspect. Adult clinical
pancreatitis is not tremendously common in the
German Shepherd Dog, but when it does occur it is
usually the middle aged, obese bitch on a fatty diet
that has it. Chronic pancreatitis symptoms include
emaciation, dull dry coat, and high appetite with
poor digestion as seen by fatty, loose stools
containing undigested starches. Treatment is aimed
mainly at correcting the diet, but it is very
difficult to control.
Pancreatic atrophy —
On the other hand, German Shepherd Dogs seem to have
a considerable predisposition to pancreatic atrophy,
also known as juvenile atrophy or pancreatic
insufficiency (PI), and certain bloodlines have been
much more associated with it than others. For years
I have referred to the milder manifestations as
subclinical pancreatitis, because people who are not
familiar with familial and breed tendencies are
likely to miss the subtle signs, and I had suspected
the two forms were variations of one basic problem.
The disease usually starts before the dog is one
year old, though many are three before symptoms are
noticed. When lack of “drive”, diminished coat
lustre, coprophagia, and/or poor weight are seen,
have the stool examined by your veterinarian for
abnormal fat level and absence or low level of the
trypsin enzyme. If the problem is discovered before
it becomes severe and chronic, Viokase™, a brand of
powdered raw pancreas, added to the food half an
hour or more before feeding usually produces good
results. Other similar products that I am familiar
with are called Pancreazyme™ and Prozyme™. I have
heard of a British product called Tryplase as well.
I was told, but have not verified this, that Prozyme
“is not the medication of choice as it only contains
the vegetable type enzymes.” Costs vary widely among
these. Getting enough to do the job without making
the owner go broke is a tough balancing act, though.
By the way, these types of preparations also appear
to be good for non specific diarrhea. I believe
there is a strong possibility that subclinical
pancreatitis can worsen with neglect into an acute
attack by enzymes on the pancreatic and surrounding
tissues themselves, and that this condition may be
the cause of many instances of diagnosed perforated
ulcers. Texas A&M vet school at one time was trying
to get AKC and GSDCA funding to study and possibly
identify a genetic marker for pancreatic acinar
atrophy in the breed.
The Animal Health
section of HelpLine (UK), autumn 1999 issue had
several articles on frank pancreas insufficiency and
malabsorption. That reported on a test for the
specific detection of pancreatic insufficiency,
using a trypsin method (TLI) from a single blood
sample. This replaced the fecal test, which had
proved inaccurate. Differential diagnosis of
pancreatic insufficiency and other small intestine
disease are sometimes difficult since clinical signs
can be similar. Many problems that befall the GSD
point to autoimmune conditions; research was carried
out by Dr. D. Williams in the U.K. Pedigrees have
been requested by veterinarians working on this
problem, and a clearinghouse for information has
been set up by Dorothy Cullum, 15 North Road,
Brentwood, Essex, England. Chronic intestinal
disease, called overgrowth of intestinal bacteria in
the UK, and probably the same thing that the U.S.’
Dr. Chuck Kruger dubbed “toxic gut syndrome”, is
also being studied in Britain, and has been found to
be a particular problem in young dogs. Treatment
with high dosage of antibiotics over a long term has
been claimed to have a good success rate.
Malabsorption or poor
digestion and stool condition are frequently seen in
the GSD, and in my experience, has been more so in
the heavily linebred typical lines in American-bred
dogs since the 1970s. These symptoms can be caused
or exacerbated by physical or emotional stress,
change of food, and other things. I suspect that
dogs with subclinical weakness in immune systems or
pancreatic function may be most likely to show these
reactions. I know that my strongest-character dogs
over the years have also been able to eat almost
anything without diarrhea. Others have also
proffered the theory of an abnormality in the immune
system. Such dogs are apparently more likely to show
symptoms like increased susceptibility to bacteria,
intolerance to change in diets, ravenous appetite,
reduction in body weight or failure to gain,
diarrhea, greasy-looking feces with possibly
undigested cellulose as well, and an “unthrifty” dry
coat. The usual response by breeders and vets is to
try the enzyme supplements and/or something like
Hills Prescription Diet. But there are about as many
stories of failure as there are of successful
(though tricky, difficult) control. Some believe
that an increase in roughage or “bulk” is needed in
order to “keep the food in the system” long enough
for the digestive system to do its work, but others
say that more bulk or roughage tends to move the
contents along a little faster. Also, we are told to
feed our affected dogs low-fat foods.
Some owners with
access to slaughterhouses claim some benefit from
feeding raw pancreas, but there is not enough data
with scientific controls to consider this anything
more than anecdotal testimony. This is not to
discount testimonials, though, as these can lead to
success and may be incentive for scientific
corroboration. One reader in the UK tried the
natural pig pancreas plus roughage route, and said,
“It [pancreas from the abattoir] is no more
unpleasant to handle than any other meat from the
freezer, costs half the price of powdered enzymes,
the dog absolutely loves it and appears to be more
effective than any man made preparation on the
market! He is not requiring as much food, as he is
obviously absorbing what he needs from his diet now.
He is not full of wind, and he is now producing
approx. 1/3 of the amount of faeces that he did on
the powders. I have also noticed that he is no
longer ravenously hungry and has actually left some
of his dinner on a few occasions.” On the other
hand, many experts say that you should reduce the
amount of non-digestible fiber in the diet for dogs
with pancreas problems.
If you choose the
expensive specialized EPI diet foods from Hills,
Eukanuba, or others, check the labels and prices —
they are “out of sight”. People who treat their EPI
dogs for the rest of the dogs’ lives can spend about
$1,000 to $1,500 annually for the enzymes alone. If
you go along this road, you will have to “soak” the
ration for a while, to give the enzymes time to work
— longer for the dry rations than for the canned.
The enzymes have their greatest effect after about
20 minutes.
Warning: you can spin
your wheels for years on the abundance and infinite
variety of nutritional advice. Many claims are
entirely unrelated and coincidental to results, but
people who are desperate will tend to try them all.
One correspondent told me that, after initial help,
she was no longer getting satisfaction by using just
the enzymes; her dog’s stools were getting poor
again. Later, she found good maintenance results by
supplementing with folate, vitamin B-12, banana,
live-culture yogurt, oatmeal, baked yams, and
flaxseed oil twice a day, in addition to “one
Cimitadine tablet (brand name is Tagamet) morning
and evening three times a week”. (Cephaloxin 500mg
two or three times daily, depending on the
situation, is sometimes administered for two weeks.)
This diet change had followed the Texas A&M College
of Vet Medicine’s suggested treatment with
cobalamine folate. Cobalamine is vitamin B-12, and
folic acid (obtained synthetically or in liver,
green leaves, and yeast) is essential to the
friendly lactobacillus in the gut, in combination
with which it inhibits malabsorption. That lady did
not see a turn-around in condition until more B-12
was added to the vet school’s recommended treatment.
She found that 2,000 milligrams of folate and a
fourth-teaspoonful of liquid B-12 with the dog’s
light meals three times a day gave marked
improvement It appears that occasional (quarterly,
for example) antibiotic treatment to kill unfriendly
bacteria, followed by folate and yogurt to encourage
the lactobacillus, is highly thought of by
veterinary nutritional specialists. I am a fan of
vitamin E, having seen benefits in many areas, so I
always recommend that people also give one or two
400-IU capsules a day of Vitamin E to help boost the
immune system.
Most people make a
distinction between EPI (Exocrine Pancreatic
Insufficiency) and pancreatitis, some saying that
dogs can recover from pancreatitis, rather simple
inflammation of the pancreas, and that when the
pancreas begins to atrophy, the only thing you can
do is supplement with digestive enzymes like Viokase
V or with Pancreazyme. I tend to believe the two
conditions are more intrinsically linked. Canned dog
foods, even the non-prescription brands, are said to
be easier for the EPI dogs to digest than is dry
kibble. The EPI dog is unable to efficiently digest
carbohydrates, protein and especially fat. The
condition is also called acinar atrophy, the word
“acinar” referring to the physical tissue structures
that make up lobules in the gland. When the pancreas
atrophies, it loses ability to function in its
digestive mode; it apparently does not interfere
with insulin production, which is its endocrine
function carried on by different types of cells.
Some dogs do become diabetic as well, but this may
be entirely unrelated.
I have been told that
the statistics on EPI dogs indicated that 1 in 5
pups born to an EPI-affected dam would eventually
show signs of EPI. There seem to be a higher than
average number of stillborn pups, as well. Whether
this has anything directly (genetically) to do with
EPI, or is a reflection on the poorer physical
condition that leads to uterine inertia, is hard to
say. By the way, on this website you are now
surfing, you might also find my article on uterine
inertia and the use of oxytocin.
The test that your vet
or his contracted lab will perform will give you a
reading of what is called Tli. This is an enzyme
blood test that determines the level of digestive
enzymes present. It can vary from day to day,
increasing and decreasing and varying within the
same day. The scale on this test from low to high,
is 5.0 to 35.0 while GSD’s rarely test over the 5.0
to 8.0 range. At Texas A&M, the Researcher told me
that they have found that dogs that normally test
below 8.0 will most probably become EPI positive. Of
course they are talking about all breeds, and we
must remember that there are breed differences. The
GSD, for example, has a higher packed-cell volume
than other breeds, and it is likely the Tli range
that is abnormal for others might be more normal for
GSDs. The disorder might remain fairly unnoticed or
asymptomatic until it reaches a Tli much below 5.0,
then the dog typically begins to get voraciously
hungry and has terrible diarrhea with a sour odor,
many times a day. Severe weight loss is an
indication that the dog is starving to death. The
fur loses pigment and gloss, becomes dry and brittle
and often is lost to some extent, and Staphylococcus
infection scabs may appear on the skin, because the
compromised immune system doesn’t allow the dog to
fight off the infection. The symptoms of EPI mostly
show up when the TLi is down around 2.5 to 3.0. In
most breeds perhaps, any dog that tests at even an
8.0 will be at high risk for EPI. So, most dogs will
be diagnosed with EPI when Tli is at 8.0 or less,
and perhaps 0.4 or lower for GSDs. If a dog is found
to be within the normal Tli range (for GSD’s 5.0 to
8.0) but exhibits symptoms such as much flatulence,
diarrhea that is light brown/yellow to clay color
from time to time, the dog should be tested for
levels of Lipase, Protease and Amylase.
The genetics of
pancreatic disorders may confuse, because the
expressions are highly variable. Some can carry the
trait and never develop EPI, while others show
symptoms, although the genotype may be similar. The
wisest recommendation is that such dogs not be bred
as they most certainly carry the recessive gene.
They are currently looking for a “marker” in the
families of dogs they’ve been working with over the
last couple of years. Before breeding, one perhaps
should have the TLi test done, and get a hint of the
possibility of carrying the gene. If you breed two
that are carriers together, you risk as much as the
entire litter having EPI. I once bought a full
brother of a famous champion named Shiloh; My
“Harry” was a beautiful animal with excellent hips,
but he developed the pancreatic disorder and had to
be controlled as much as possible with the enzyme
powder. I had sold a co-ownership in him before the
disorder developed, and he was killed in a car crash
before years of treatment and follow-up would have
been completed. Some others with close relatives
also reported pancreatic insufficiency in their
dogs. One vet I know of told his client that EPI “is
not considered being ill — merely a genetic
condition.” Merely a matter of semantics? To me,
pancreatic insufficiency is an abnormality that
calls for removal from the gene pool, whether the
dog has a mild case or asymptomatic most of the
time. I have found that most vets take but a modicum
of hours of nutrition and practical genetics classes
in vet school, and then forget most because they
don’t use it every day. Breeders, especially those
with a science background, are more reliable sources
of information, I think. Unfortunately, not many
people who offer their EPI males at stud admit or
declare any cautions about their dogs. As one
observer quipped, “It’s funny isn’t it, that those
who deny all those things have Viokase-V on the
shelf in their back rooms?” Yes, in spite of the
fact it is good for various causes of diarrhea, it
is so much more expensive than Kaopectate, that it
makes you wonder.
Connection between PI
and GDV? — There have been reports from dog owners
indicating that many episodes of EPI begin with a
bloating incident, or with a gastroenteritis, marked
by vomiting and blood tinged diarrhea. One who had
“chatted” on the Internet with many GSD owners in
the UK and the USA said, “From the general info
collected, the dog first bloats, which often leads
to torsion of the gut, which of course requires
surgery for a tacking of the stomach, and this is
usually followed by a full blown episode of EPI
within a few months of the surgery.”
Intussusception — In
very young pups (and other animals including humans)
the intestine can invaginate (one part slips inside
another). The condition, also referred to as
“telescoping intestines”, also occurs in adults, but
not as frequently. Most common immediate causes
include worms, obstruction by indigestible
materials, garbage, or toxic substances. The German
Shepherd seems to experience a high incidence of
this disorder and I believe there is a genetic
propensity, a familial trait, in certain bloodlines.
Diarrhea and soft
stool — Diarrhea can be a symptom of any number of
disorders from cancer to overeating, but is most
often associated with disease or parasitism of the
small intestine. Diarrhea or loose stool is quite
common in the German Shepherd Dog, even when no
physiological disease has been identified. However,
since this is not a normal condition, the owner
should make a sincere attempt to find and attack the
cause. Some of the causative factors in true
diarrhea are: pancreatic insufficiency, chemical or
mechanical irritation of intestinal linings,
parasites, microorganisms, and a psychosomatic
condition related to the “high-strung,” emotional
make-up of the German Shepherd Dog. Foods that can
cause loose stool include milk (if suddenly
introduced into the diet), excessive liver, fats,
and those with a high fiber content. However, simple
overeating is perhaps the most frequent culprit.
Most people overfeed their dogs.
Soft to runny stools
may be an indication of a general inflammation of
the stomach and intestines known as eosinophilic
gastroenteritis. It is treated symptomatically with
something to coat the lining, plus perhaps a steroid
and Kaopectate, until the dog “heals itself.” Many
veterinarians and owners administer Pepto-Bismol,
also. In the case of very young puppies with watery
stool or repeated diarrhea, rush to your veterinary
clinic with the pup and the stool samples. Most of
the time the cause of diarrhea in a young puppy is
serious, such as parvo or coccidiosis, perhaps with
hookworm as well. The Campylobacter bacteria cause
some cases of acute or chronic diarrhea, and most
labs would have no trouble identifying this
infection. Generally watery diarrhea is not an
indicator of “campy”. Erythromycin antibiotic is 90%
effective, although resistant strains may be
evolving.
Even giardia can be
quite dangerous, if the pup is young and has been
exposed to other challenges, such as being wormy,
stressed, or otherwise weakened. Giardiasis is
marked by watery diarrhea with a uniquely acrid
“bloody” odor, that experienced breeders can
identify quite easily even before a stool sample is
analyzed. Giardia is a protozoan disease; i.e., it
is caused by a single-celled “animal” flagellate
parasite, so-called because it is highly motile,
having a tail. The Merck Veterinary Manual describes
it: “Transmission occurs in the cyst stage by the
fecal-oral route. Incubation and pre-patent periods
are generally 5 to 14 days. Giardia cysts survive in
the environment and thus are a source of infection
and reinfection for animals, particularly those in
crowded conditions... prompt removal of feces from
cages, runs, and yards will limit environmental
contamination. Cysts contaminating the hair of dogs
and cats may be a source of reinfection.” Regarding
treatment, the manual says “Flagyl ™ (metronidazole)
is about 65% effective” (in removing cysts from
feces) and if administered “for 3 days, effectively
removes giardia cysts from feces of dogs; no side
effects are reported.” By the way, these oocysts are
much smaller than worm eggs, and require much higher
magnification to find them; still, they are not shed
every day, so it may be wise to start treatment and
then wait for a three-to-five-day combined stool
sample to be checked by your vet. Despite the “low”
rate or ridding the body of cysts, many vets prefer
Flagyl. The success rate is reportedly declining as
giardia is now demonstrating resistance to the drug.
In addition, it may be a little hard on young
puppies, with some neurological side effects.
Panacur (fenbendazole)
is relatively pricey and seems to be sold only in
large-volume jars from the usual vet supply
catalogs. For giardia, Panacur is considered a
static drug, 100% effective in clearing cysts from
feces in 3 days (the cysts are the infective part),
with no side effects reported, and is safe for
pregnant and lactating animals. In the lab, giardia
did not develop resistance to fenbendazole. It does
not have a repelling taste. A field representative
for Intervet, the company that manufactures Panacur,
admitted that Flagyl may be preferable for the
occasional dog that has general stomach distress.
With either one, a 5-day dose has been reported by
some to be effective when the 3-day regime was not.
I would also recommend
that you ask your vet about Albon™ (sulfamethoxine)
which is much more effective, although for a
different reason, and should be given for 15 to 21
days. The sulfa drugs do nothing to the Giardia
organism itself, but they do combat the secondary
bacterial infections that are probably the real
killers of puppies. Such an approach allows the pup
to regain enough health to withstand the protozoan,
even though it may be retained in the body for a
while. It is more readily available, probably lower
in cost, and in widespread use. A disadvantage in
any sulfa drug is a number of adverse side-effects,
but I have not had any problems, probably because I
do not keep dogs on the medication longer than
recommended, and have genetically strong breeding
stock.
There are a few
less-often used: Valbazen (albendazole) is about 90%
effective in removing cysts but has been implicated
in birth defects, suppression of the immune system,
and destruction of red blood cells. .Atabrine
(quinacrine) also has unpleasant side effects. Some
have recommended a Giardia Lamblia vaccine for dogs
with persistent or repeated cases.
Toxic gut syndrome (TGS)
— This disorder has been identified as a specific
syndrome, with some similarities to other disorders
such as intestinal volvulus, which may have been
blamed for death when TGS was the real villain. The
German Shepherd Dog has a higher packed cell volume
(number of blood cells per unit of blood) than do
most other breeds, with 50 to 60 percent “solids”
compared with 40 to 45 percent. When such a dog
becomes dehydrated, thickened and/or lessened blood
supply to the small intestine increases growth of
bacteria that are always present there. These
Clostridium and E. cold bacteria produce such
quantities of toxins that the dog is unable to get
rid of them fast enough, and death by poisoning
occurs. By the time owners see symptoms such as
discomfort when the abdomen is touched, attempts to
vomit, and excessive salivation, it is probably too
late. Prevention may be accomplished through dietary
means (feeding Lactobacillus acidophilus, yogurt, or
cultured buttermilk), or by the same toxoid vaccine
that is given to lambs to prevent Clostridium
perfringens types C and D. As research is done on
this recently defined syndrome, more will become
known as to the best treatment.
Other problems —
Ulcers have been diagnosed too frequently in German
Shepherds and may be related to pancreatic problems
or other causes: it’s difficult to tell, when
several conditions exist at once, whether one is the
cause or effect of another. Necrotic bowel syndrome,
a disorder of unknown cause, is diagnosed usually on
autopsy, when part of the intestine is found to be
dead and rotting away. This condition may be
synonymous with or overlap intussusception or other
diseases. It takes a small toll, mostly among
heavily linebred German Shepherd Dogs.
Eosinophilic
ulcerative colitis — This syndrome is most common in
Cocker Spaniels and German Shepherd Dogs. If your
pup or adult has intermittent to constant diarrhea,
with or without blood, and does not respond to
treatments for the more common disorders, this
disease may be the cause. Initial treatment may
include corticosteroids, antibiotics, and
antispasmodics to see if the symptoms can be halted.
Irritable colon — Also
known as spastic colon, this disorder with mucus in
or on the surface of soft or frequent stools may be
the result of stress. The best cure is prevention —
breed stable temperaments and build confidence in
puppies.
Polyps — Rectal polyps
are little round or teardrop shaped red to purplish
balls. Sometimes they are clustered like tiny
grapes, and are found very close to the anal opening
or further inside the rectum. They should be
surgically removed, since they rupture easily and
are a potential site for infection. A drop of bright
red blood recurring on the end of stools is a sign
that you should have the dog examined for polyps.
****************************************************
The author is a breeder since 1945, a teacher and
lecturer in canine topics, and dog show judge. His
book, The Total German Shepherd Dog, is available
from
http://www.Hoflin.com and he can be contacted at
Mr.GSD@Juno.com |